Pediatric Neurologist FAQs
Concerned parents understandably have a litany of questions regarding pediatric neurology, what pediatric neurologists do and how they are trained, and, most importantly, how to find the best care for their child in their hour of need.
Let’s get into the most frequently asked questions (FAQs) regarding pediatric neurology.
What is a pediatric neurologist?
Neurology is the field of medicine that focuses on treating health conditions associated with the nervous system, which includes the brain, nerves, and spinal cord.
“Pediatric” means “of or pertaining to the medical care or diseases of children.”
Therefore, pediatric neurology refers to medicine focused on treating and optimizing children’s nervous system function.
What nervous system conditions do pediatric neurologists treat?
Children’s brains and nerves can be impacted by a wide array of health conditions, both acute and chronic. Accordingly, pediatric neurologists treat a broad range of conditions. Examples of common neurological issues that neurologists treat include:
- epilepsy and other seizure disorders
- movement disorders
- infections of the brain
- autism
- cerebral palsy
- multiple sclerosis
- traumatic brain injury
- stroke
- attention deficit disorders
Like other doctors, many pediatric neurologists specialize in the treatment of one particular neurological condition, or a small handful of tightly related conditions, such as cerebral palsy and related movement disorders.
What training do pediatric neurologists undergo?
In total, becoming a practicing, licensed child neurologist requires an average of 12-13 years of training.
The pediatric neurologist’s training follows this general trajectory:
- 4 years of undergraduate work. Here, the college student studies physics, biology, anatomy, chemistry, and physiology, in addition to other, more general subjects.
- 4 years of medical school. This typically includes two years of in-class instruction and two years of supervised clinical practice.
- One-to-two-year internship in pediatrics. Following graduation from medical school, new graduates perform more rigorous hands-on practice in their chosen specialty with an internship.
- Three-year residency in child neurology. After completing an internship, the next step is to enroll in a residency program in a clinic or hospital treating children with neurological issues. During residency, senior, seasoned child neurologists mentor their younger counterparts to instill a strong practical knowledge base to draw on in their future work.
Given the enormous stakes, requiring child neurologists to undergo such a rigorous training regimen to earn their positions is understandable and necessary to ensure optimal care for vulnerable patients in their greatest hour of need.
What are the licensing requirements for pediatric neurologists?
Before entering into clinical practice, pediatric neurologists must pass the United States Medical Licensing Examination (USMLE) license, a baseline requirement for all physicians who treat patients in the US.
In some states, neurologists may also need American Board of Psychiatry and Neurology (ABPN) certification.
What clinical tests do pediatric neurologists perform?
Modern medicine provides multiple tools to accurately assess a patient’s neurological function. These include:
- Blood tests. Blood samples can be used to detect important markers of nervous system health, such as inflammation levels, genetic conditions using DNA analysis, and infections from bacteria, viruses, or other pathogens.
- MRI (magnetic resonance imaging). Powerful magnets and radio waves create high-resolution images of nervous system tissue.
- CT (computerized tomography) scans. High-definition x-rays take multiple snapshots of the brain from different angles to produce a 3D profile.
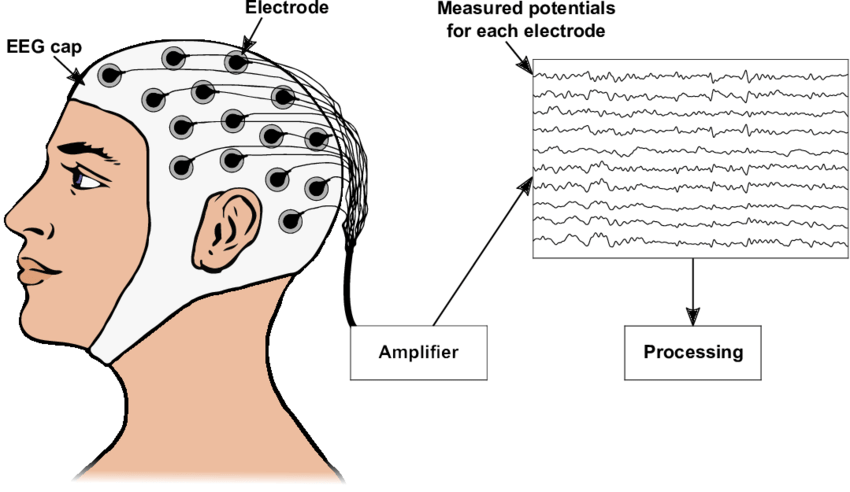
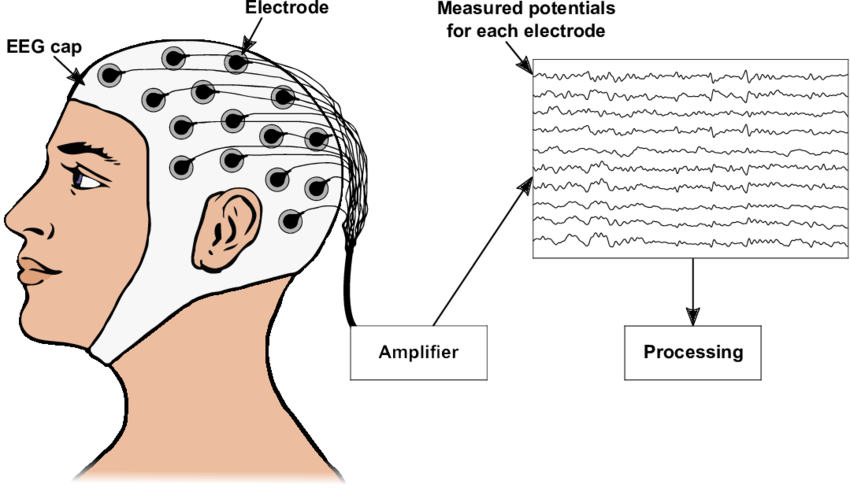
- EEG (electroencephalogram). In this noninvasive procedure, a series of sensors called electrodes are placed on the surface of the brain and brain stem to detect and record nervous system electrical activity.
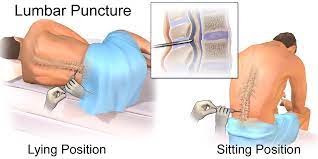
- Lumbar puncture (aka “spinal tap”). A small sample of cerebrospinal fluid (CSF) is collected from the spine for analysis to diagnose meningitis, encephalitis, and other neurological conditions in children.
- Positron emission tomography (PET) scans. Harmless radioactive isotopes called “tracers” are introduced to the bloodstream to produce an image that shows blood flow and neurological tissue metabolism, as well as detecting tumors.
For a more complete exploration of the technologies that neurologists rely on to make accurate diagnoses and monitor patients’ progress throughout treatment, please visit our authoritative blog post on that topic.
Where do pediatric neurologists work?
Pediatric neurologists operate in a variety of contexts and at various locations. The most common places where child neurologists work include:
- children’s hospitals
- clinics
- public health foundations
- research institutes
- university medical centers
- community-based outpatient practices
- private offices
Nervous system disorders in children are often complex, involving other systems and organs of the body like the heart, liver, kidneys, or lungs. Depending on the root cause of the symptoms, there might be additional complications of the condition.
To address such complex challenges, pediatric neurologists frequently collaborate with other specialists, drawing on their unique expertise to develop optimal healthcare solutions for patients. The types of doctors that might partner with pediatric neurologists on a case-by-case basis include:
- Pediatric Endocrinologist (Gland/Hormone Doctor)
- Developmental/Behavioral Pediatrician (Developmental/Behavioral Doctor)
- Pediatric Radiologist
- Pediatric Oncologist (Cancer Doctor)
- Neonatologist (Preemie Doctor)
- Pediatric Cardiologist (Heart Doctor)
- Pediatric Otolaryngologist (Ear, Nose and Throat Doctor – ENT)
Pediatric neurologists’ role in public health policy
Most pediatric neurologists spend the majority of their careers treating patients. Others, however, either on a volunteer or paid basis, either full-time or part-time, also do important work in the public health policy field.
The objective of public health policy is to maximize the health benefits to the highest numbers of patients by organizing and developing resources within the health system in order to best serve the needs of the population at the administrative level.
Although public health policy, which focuses on the macro level, might seem abstract, it is actually critical to enhancing the patient experience at the micro level in clinical practice.
How much do pediatric neurologists earn?
Most pediatric neurologists earn, on average, $175,000-$350,000 per year.
Are there enough pediatric neurologists working in the US to meet patient needs?
The US needs more pediatric neurologists. According to the Child Neurology Foundation, there are 20% fewer pediatric neurologists currently working in clinics than required to meet the national need.
Are men or women more likely to become pediatric neurologists?
More women are pediatric neurologists than men. Broken down by gender, about 65% of pediatric neurologists are female and 35% are male.
What documents should parents bring to a pediatric neurology appointment?
Optimal treatment – getting an accurate diagnosis and developing an effective treatment plan — depends on gathering the most information possible. Accordingly, parents/guardians should bring all relevant documents, including previous test results, other doctors’ notes, and even report cards from school to the appointment.
In addition, for a streamlined administrative process, parents should also bring their child’s insurance card and a parent’s photo ID.
Where can the public go to learn more about pediatric neurologists?
If you have more questions regarding pediatric neurology, its practice, and the doctors who work in this field, consider utilizing the following authoritative resources:
- Child Neurology Foundation
- ACGME
- Child Neurology Society
- American Board of Psychiatry and Neurology
- American Academy of Neurology Child Neurology Section
- American Academy of Pediatrics Section on Neurology
- American Board of Pediatrics
- NRMP
Contact Child Neurology Center of Northwest Florida to learn more
For more answers to your most pressing questions concerning this field of medicine, don’t hesitate to contact Child Neurology Center of Northwest Florida.